
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- Drug/Regimen
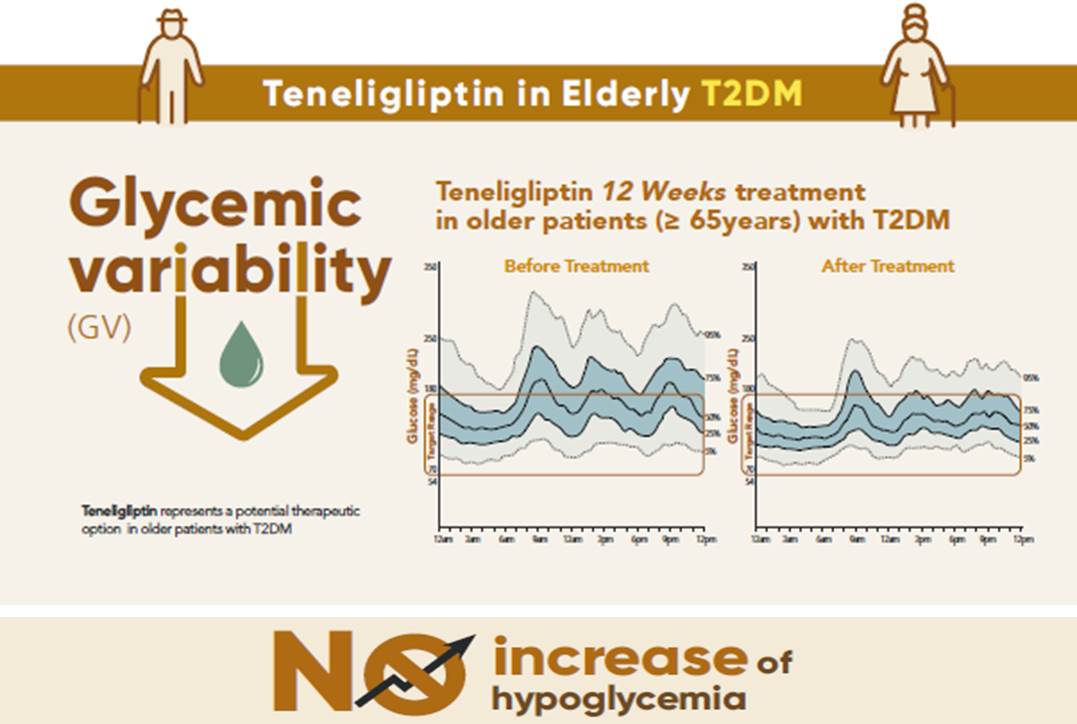
- Effects of Teneligliptin on HbA1c levels, Continuous Glucose Monitoring-Derived Time in Range and Glycemic Variability in Elderly Patients with T2DM (TEDDY Study)
- Ji Cheol Bae, Soo Heon Kwak, Hyun Jin Kim, Sang-Yong Kim, You-Cheol Hwang, Sunghwan Suh, Bok Jin Hyun, Ji Eun Cha, Jong Chul Won, Jae Hyeon Kim
- Diabetes Metab J. 2022;46(1):81-92. Published online June 16, 2021
- DOI: https://doi.org/10.4093/dmj.2021.0016
- 7,595 View
- 431 Download
- 5 Web of Science
- 5 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub 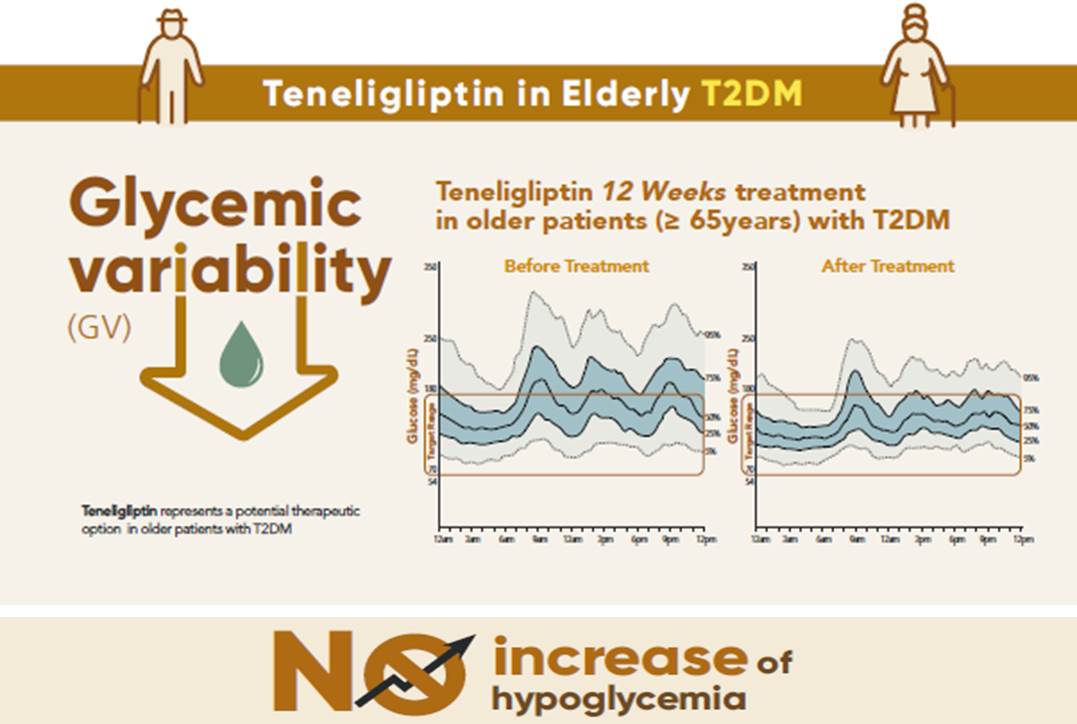
- Background
To evaluate the effects of teneligliptin on glycosylated hemoglobin (HbA1c) levels, continuous glucose monitoring (CGM)-derived time in range, and glycemic variability in elderly type 2 diabetes mellitus patients.
Methods
This randomized, double-blinded, placebo-controlled study was conducted in eight centers in Korea (clinical trial registration number: NCT03508323). Sixty-five participants aged ≥65 years, who were treatment-naïve or had been treated with stable doses of metformin, were randomized at a 1:1 ratio to receive 20 mg of teneligliptin (n=35) or placebo (n=30) for 12 weeks. The main endpoints were the changes in HbA1c levels from baseline to week 12, CGM metrics-derived time in range, and glycemic variability.
Results
After 12 weeks, a significant reduction (by 0.84%) in HbA1c levels was observed in the teneligliptin group compared to that in the placebo group (by 0.08%), with a between-group least squares mean difference of –0.76% (95% confidence interval [CI], –1.08 to –0.44). The coefficient of variation, standard deviation, and mean amplitude of glycemic excursion significantly decreased in participants treated with teneligliptin as compared to those in the placebo group. Teneligliptin treatment significantly decreased the time spent above 180 or 250 mg/dL, respectively, without increasing the time spent below 70 mg/dL. The mean percentage of time for which glucose levels remained in the 70 to 180 mg/dL time in range (TIR70–180) at week 12 was 82.0%±16.0% in the teneligliptin group, and placebo-adjusted change in TIR70–180 from baseline was 13.3% (95% CI, 6.0 to 20.6).
Conclusion
Teneligliptin effectively reduced HbA1c levels, time spent above the target range, and glycemic variability, without increasing hypoglycemia in our study population. -
Citations
Citations to this article as recorded by- Comparison of teneligliptin and other gliptin-based regimens in addressing insulin resistance and glycemic control in type 2 diabetic patients: a cross-sectional study
Harmanjit Singh, Ravi Rohilla, Shivani Jaswal, Mandeep Singla
Expert Review of Endocrinology & Metabolism.2024; 19(1): 81. CrossRef - Potential approaches using teneligliptin for the treatment of type 2 diabetes mellitus: current status and future prospects
Harmanjit Singh, Jasbir Singh, Ravneet Kaur Bhangu, Mandeep Singla, Jagjit Singh, Farideh Javid
Expert Review of Clinical Pharmacology.2023; 16(1): 49. CrossRef - Mechanism of molecular interaction of sitagliptin with human DPP4 enzyme - New Insights
Michelangelo Bauwelz Gonzatti, José Edvar Monteiro Júnior, Antônio José Rocha, Jonathas Sales de Oliveira, Antônio José de Jesus Evangelista, Fátima Morgana Pio Fonseca, Vânia Marilande Ceccatto, Ariclécio Cunha de Oliveira, José Ednésio da Cruz Freire
Advances in Medical Sciences.2023; 68(2): 402. CrossRef - A prospective multicentre open label study to assess effect of Teneligliptin on glycemic control through parameters of time in range (TIR) Metric using continuous glucose monitoring (TOP-TIR study)
Banshi Saboo, Suhas Erande, A.G. Unnikrishnan
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2022; 16(2): 102394. CrossRef - Association between Variability of Metabolic Risk Factors and Cardiometabolic Outcomes
Min Jeong Park, Kyung Mook Choi
Diabetes & Metabolism Journal.2022; 46(1): 49. CrossRef
- Comparison of teneligliptin and other gliptin-based regimens in addressing insulin resistance and glycemic control in type 2 diabetic patients: a cross-sectional study
- Epidemiology
- Clinical Characteristics of People with Newly Diagnosed Type 2 Diabetes between 2015 and 2016: Difference by Age and Body Mass Index
- Kyoung Hwa Ha, Cheol Young Park, In Kyung Jeong, Hyun Jin Kim, Sang-Yong Kim, Won Jun Kim, Ji Sung Yoon, In Joo Kim, Dae Jung Kim, Sungrae Kim
- Diabetes Metab J. 2018;42(2):137-146. Published online February 14, 2018
- DOI: https://doi.org/10.4093/dmj.2018.42.2.137
- 5,376 View
- 80 Download
- 11 Web of Science
- 11 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background We evaluated the clinical characteristics of insulin resistance and β-cell dysfunction in newly diagnosed, drug-naive people with type 2 diabetes by analyzing nationwide cross-sectional data.
Methods We collected the clinical data of 912 participants with newly diagnosed diabetes from 83 primary care clinics and hospitals nationwide from 2015 to 2016. The presence of insulin resistance and β-cell dysfunction was defined as a homeostatic model assessment of insulin resistance (HOMA-IR) value ≥2.5 and fasting C-peptide levels <1.70 ng/mL, respectively.
Results A total of 75.1% and 22.6% of participants had insulin resistance and β-cell dysfunction, respectively. The proportion of participants with insulin resistance but no β-cell dysfunction increased, and the proportion of participants with β-cell dysfunction but no insulin resistance decreased as body mass index (BMI) increased. People diagnosed with diabetes before 40 years of age had significantly higher HOMA-IR and BMI than those diagnosed over 65 years of age (HOMA-IR, 5.0 vs. 3.0; BMI, 28.7 kg/m2 vs. 25.1 kg/m2). However, the β-cell function indices were lower in people diagnosed before 40 years of age than in those diagnosed after 65 years of age (homeostatic model assessment of β-cell function, 39.3 vs. 64.9; insulinogenic index, 10.3 vs. 18.7; disposition index, 0.15 vs. 0.25).
Conclusion We observed that the main pathogenic mechanism of type 2 diabetes is insulin resistance in participants with newly diagnosed type 2 diabetes. In addition, young adults with diabetes are more likely to have higher insulin resistance with obesity and have higher insulin secretory defect with severe hyperglycemia in the early period of diabetes than older populations.
-
Citations
Citations to this article as recorded by- A double‐blind, Randomized controlled trial on glucose‐lowering EFfects and safety of adding 0.25 or 0.5 mg lobeglitazone in type 2 diabetes patients with INadequate control on metformin and dipeptidyl peptidase‐4 inhibitor therapy: REFIND study
Soree Ryang, Sang Soo Kim, Ji Cheol Bae, Ji Min Han, Su Kyoung Kwon, Young Il Kim, Il Seong Nam‐Goong, Eun Sook Kim, Mi‐kyung Kim, Chang Won Lee, Soyeon Yoo, Gwanpyo Koh, Min Jeong Kwon, Jeong Hyun Park, In Joo Kim
Diabetes, Obesity and Metabolism.2022; 24(9): 1800. CrossRef - Apparent Insulin Deficiency in an Adult African Population With New-Onset Type 2 Diabetes
Davis Kibirige, Isaac Sekitoleko, Priscilla Balungi, William Lumu, Moffat J. Nyirenda
Frontiers in Clinical Diabetes and Healthcare.2022;[Epub] CrossRef - Rising Incidence of Diabetes in Young Adults in South Korea: A National Cohort Study
Hyun Ho Choi, Giwoong Choi, Hojun Yoon, Kyoung Hwa Ha, Dae Jung Kim
Diabetes & Metabolism Journal.2022; 46(5): 803. CrossRef - A Real-World Study of Long-Term Safety and Efficacy of Lobeglitazone in Korean Patients with Type 2 Diabetes Mellitus
Bo-Yeon Kim, Hyuk-Sang Kwon, Suk Kyeong Kim, Jung-Hyun Noh, Cheol-Young Park, Hyeong-Kyu Park, Kee-Ho Song, Jong Chul Won, Jae Myung Yu, Mi Young Lee, Jae Hyuk Lee, Soo Lim, Sung Wan Chun, In-Kyung Jeong, Choon Hee Chung, Seung Jin Han, Hee-Seok Kim, Ju-Y
Diabetes & Metabolism Journal.2022; 46(6): 855. CrossRef - The Potential Effect of Rhizoma coptidis on Polycystic Ovary Syndrome Based on Network Pharmacology and Molecular Docking
Liyun Duan, De Jin, Xuedong An, Yuehong Zhang, Shenghui Zhao, Rongrong Zhou, Yingying Duan, Yuqing Zhang, Xinmin Liu, Fengmei Lian, Wen yi Kang
Evidence-Based Complementary and Alternative Medicine.2021; 2021: 1. CrossRef - PRKAA2variation and the clinical characteristics of patients newly diagnosed with type 2 diabetes mellitus in Yogyakarta, Indonesia
Dita Maria Virginia, Mae Sri Hartati Wahyuningsih, Dwi Aris Agung Nugrahaningsih
Asian Biomedicine.2021; 15(4): 161. CrossRef - Efficacy and Safety of Pioglitazone versus Glimepiride after Metformin and Alogliptin Combination Therapy: A Randomized, Open-Label, Multicenter, Parallel-Controlled Study
Jeong Mi Kim, Sang Soo Kim, Jong Ho Kim, Mi Kyung Kim, Tae Nyun Kim, Soon Hee Lee, Chang Won Lee, Ja Young Park, Eun Sook Kim, Kwang Jae Lee, Young Sik Choi, Duk Kyu Kim, In Joo Kim
Diabetes & Metabolism Journal.2020; 44(1): 67. CrossRef - Favorable Glycemic Control with Once-Daily Insulin Degludec/Insulin Aspart after Changing from Basal Insulin in Adults with Type 2 Diabetes
Han Na Jang, Ye Seul Yang, Seong Ok Lee, Tae Jung Oh, Bo Kyung Koo, Hye Seung Jung
Endocrinology and Metabolism.2019; 34(4): 382. CrossRef - Insulin Resistance versus β-Cell Failure: Is It Changing in Koreans?
Mi-kyung Kim
Diabetes & Metabolism Journal.2018; 42(2): 128. CrossRef - Response: Clinical Characteristics of People with Newly Diagnosed Type 2 Diabetes between 2015 and 2016: Difference by Age and Body Mass Index (Diabetes Metab J2018;42:137-46)
Kyoung Hwa Ha, Dae Jung Kim, Sungrae Kim
Diabetes & Metabolism Journal.2018; 42(3): 251. CrossRef - Letter: Clinical Characteristics of People with Newly Diagnosed Type 2 Diabetes between 2015 and 2016: Difference by Age and Body Mass Index (Diabetes Metab J 2018;42:137-46)
Ah Reum Khang
Diabetes & Metabolism Journal.2018; 42(3): 249. CrossRef
- A double‐blind, Randomized controlled trial on glucose‐lowering EFfects and safety of adding 0.25 or 0.5 mg lobeglitazone in type 2 diabetes patients with INadequate control on metformin and dipeptidyl peptidase‐4 inhibitor therapy: REFIND study
- Letter: The Risk of Bladder Cancer in Korean Diabetic Subjects Treated with Pioglitazone (
Diabetes Metab J 2012;36:371-8) - Sang-Yong Kim
- Diabetes Metab J. 2012;36(6):460-461. Published online December 12, 2012
- DOI: https://doi.org/10.4093/dmj.2012.36.6.460
- 2,847 View
- 25 Download
- 1 Crossref

 KDA
KDA
 First
First Prev
Prev





